On the Amazon page for my book The Hungry Brain, the top review is positive overall but regrets that I didn’t cover the role of the gut microbiota in obesity. This reflects a common belief that differences in the microbial composition of the human gut are an important determinant of body fatness. In fact, the omission in my book was deliberate, because despite the popularity of this idea, I’m still not convinced it’s correct. In this post, I’ll review three recent findings that have added to my skepticism, including a human fecal microbiota transplant study that doesn’t mean what most people think it means. I’ll note up front that I don’t think this evidence proves that the gut microbiota isn’t involved in determining body fatness– it just proves that the hype is outpacing the science.
Finding #1
The first finding is actually a reanalysis of a seminal result in the microbiota-obesity field. The initial paper was published in the journal Nature in 2006, and to large extent, it built the field. The key experiment shows that a fecal microbiota transplant from an obese mouse to a lean (microbiota-free) mouse can make the latter gain fat. This was an important milestone because it demonstrated for the first time, apparently unequivocally, that the microbiota was actually causing part of the fattening effect– not just along for the ride. The study has been cited 5,931 times.
I’ve always been skeptical of this paper, for different reasons, but recently a microbiome researcher named Matthew Dalby took a closer look at the data underlying the claim that body fatness can be transferred via the microbiota and published the results on his blog. I won’t get into the details of his analysis– you can read them on his blog if you’re interested– but suffice it to say the finding doesn’t survive critical inquiry. The effect size is trivial and it’s likely explained by a statistical artifact called regression to the mean [Update 3/27/18: Jeffrey Walker has done a detailed statistical analysis of this experiment and shown that it is indeed likely explained by regression to the mean]. This type of anomaly is one of the hazards of using small groups of animals in your experiments (9 – 10 per group in this case), and it was exacerbated by the way the researchers chose to report the data.
This undermines a seminal finding of the microbiota-obesity field and increases my skepticism about the hypothesis as a whole.
Finding #2
The second finding is also from Matthew Dalby, but this time in the form of a study. Published late last year in Cell Reports, the study compares body fatness, metabolic health, and gut microbiome of mice fed three different diets:
- Unrefined low-fat diet. This is the typical maintenance diet for rodent colonies and it’s primarily composed of unrefined grains and soybeans.
- Refined low-fat diet. This diet is composed mostly of refined carbohydrate, largely corn starch and maltodextrin, but also a bit of sucrose. It contains casein for protein and a few other ingredients.
- Refined high-fat diet. This is the typical style of diet that’s used to produce obesity in rodents, including in my own experiments. It’s mostly lard by calories, but also contains corn starch, maltodextrin, and a bit of sucrose. It contains casein for protein and a few other ingredients.
There are many interesting findings in this paper, but for our purposes there is one key result. The mice fed the unrefined low-fat diet and the refined low-fat diet remained lean and metabolically healthy (good glucose tolerance), while the mice fed the refined high-fat diet quickly became obese and metabolically unhealthy (poor glucose tolerance)…
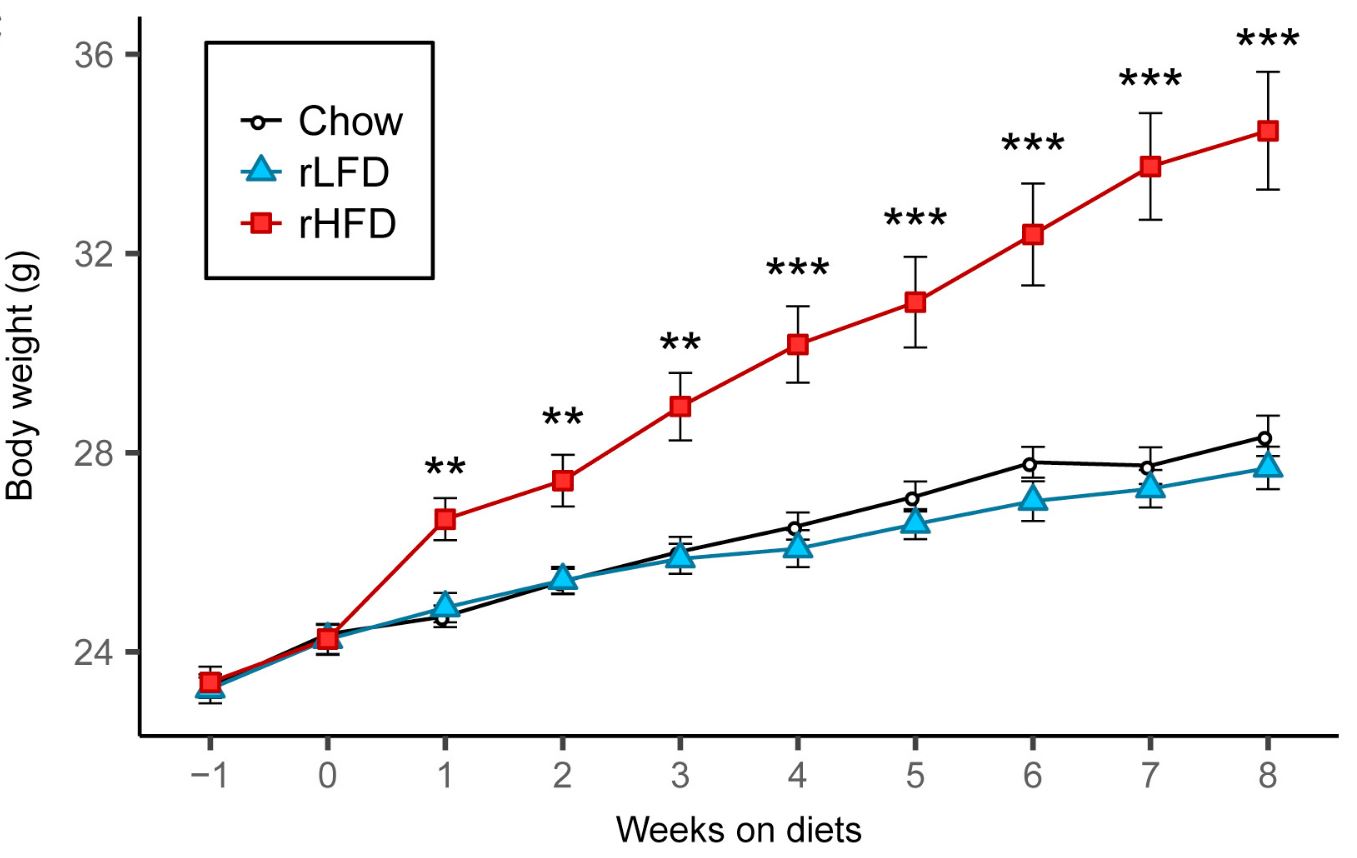
…Yet when they examined the gut microbiota, it was similar in the mice eating the refined low-fat and refined high-fat diets (while the microbiota on both refined diets were quite different from the unrefined diet). Therefore, differences in the microbial composition of the gut flora couldn’t explain differences in body fatness or metabolic health.
Finding #3, or how not to analyze data and report study results
The ultimate proof that gut microbiota impacts human body fatness would be a study demonstrating that a fecal microbiota transplant from lean people to people with obesity can cause weight loss, or vice versa. The first study to examine the weight impact of a fecal microbiota transplant from lean people to people with obesity was recently published— let’s have a look.
The first place we’ll go is to the study’s preregistration site. This is the place where the authors laid out their research plan prior to conducting the study, including how the data would be analyzed an interpreted. The reasons authors preregister research plans, aside from the fact that it’s often required by quality journals, is that it shows that they didn’t tweak their analysis and reporting after seeing the data, in order to engineer a preferred outcome. This can lead to results that are convenient for the researchers but misleading for the scientific community. Preregistration is a critically important tool for combating the “replication crisis” that is currently sweeping many fields of research as we realize their findings aren’t as reliable as we thought they were.
One of the most important things a researcher should preregister in any randomized trial is the study’s “primary outcome”. This is the outcome that will matter the most for study design, data analysis, and interpretation. It is the outcome that researchers commit in advance to focusing on in the resulting publication, no matter what the results are. Researchers can also register “secondary outcomes”, which are less important. In this case, the preregistered primary outcome was “changes in weight in relation to fecal flora composition and short chain fatty acid metabolism in fecal samples after 3, 6, 12 and 18 weeks”. This isn’t very specific but it’s clear that the primary outcome is about changes in body weight. Thus, according to the researchers themselves, the study was designed and committed in advance to be primarily about body weight. Insulin resistance is listed as a secondary outcome.
Onward to the paper. The title should immediately send up a red flag: “Improvement of Insulin Sensitivity after Lean Donor Feces in Metabolic Syndrome Is Driven by Baseline Intestinal Microbiota Composition”. The title focuses on a secondary outcome but doesn’t mention the primary outcome of body weight, and the abstract does the same. In fact, the paper barely mentions that the intervention had no impact on body weight at the two reported time points of 6 and 18 weeks, and all the figures relating to it are in the supplementary materials. Let’s not be misled by this sleight of hand: the study was primarily about the impact of fecal microbiota transplant on body weight, and it found no effect.
The paper does claim that lean microbiota improved insulin sensitivity at 6 weeks, but this result is unconvincing due to poor statistical methods. I’ll relegate my discussion of this to a footnote so I don’t bore you with technical details.* I don’t know what the reviewers were smoking while reading this paper but it must have been strong stuff.
Conclusion
We still don’t have compelling evidence that differences in the composition of the gut microbiota significantly impact body fatness in humans, and the best human evidence we have suggests that it may not be important. New evidence also suggests that it may not be as important in rodents as we thought either. That said, the case isn’t closed yet. The human evidence we have is short-term, and given the staggering complexity of the microbiota and how it interacts with diet and lifestyle, there is still room for it to be important. I look forward to further research on it, but in the meantime, let’s cut back on the hype.
Thanks to Matthew Dalby for his thoughts on this post.
* They used within-group comparisons to show that the group receiving the lean-type microbiota showed increased insulin-mediated glucose uptake over the 6-week period, but the control group didn’t. They interpreted this as showing that the fecal transplant improved insulin sensitivity. The problem with this is that key statistical tests in randomized controlled trials have to directly compare between groups, not within groups. Otherwise, why bother having a control group?